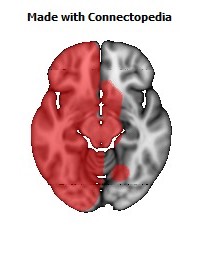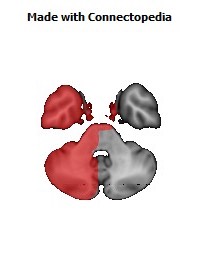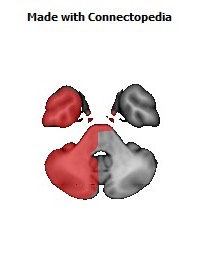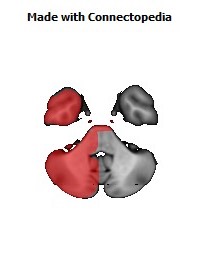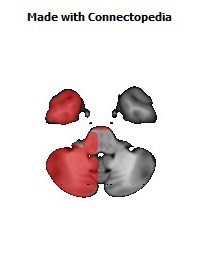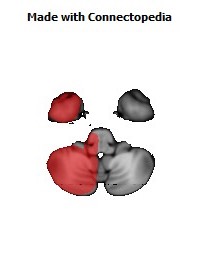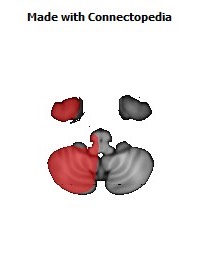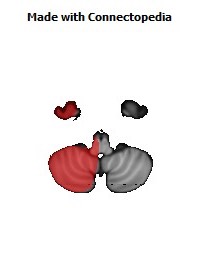
Internal jugular vein is a paired vein collecting the blood from the brain, the superficial parts of the face, and the neck. An internal jugular vein is a type of jugular vein.
Path
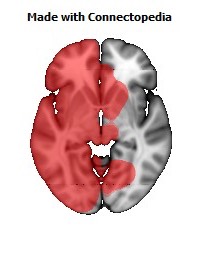
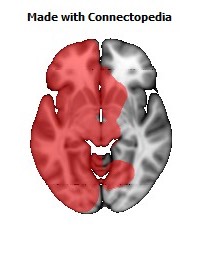
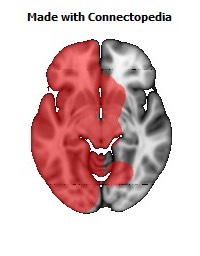
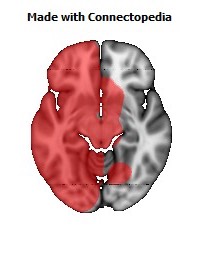
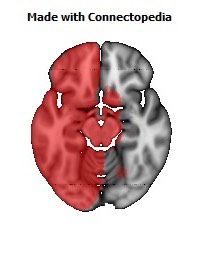
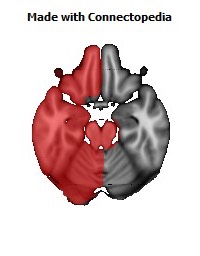
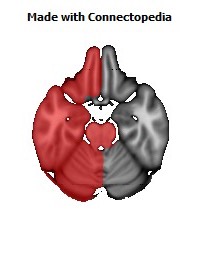
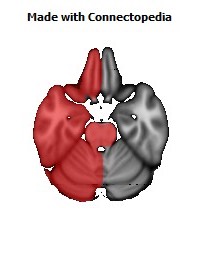
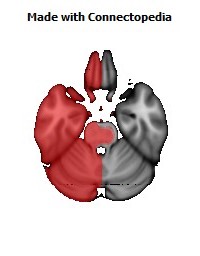
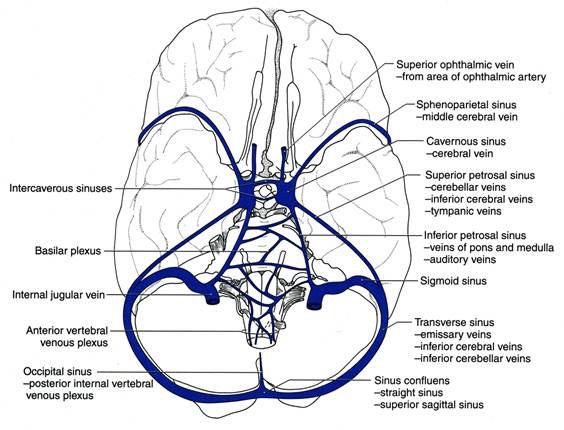
On both sides and at the base of the brain, the inferior petrosal sinus and the sigmoid sinus join to form the internal jugular vein. The internal jugular vein begins in the posterior compartment of the jugular foramen, at the base of the skull.
It is somewhat dilated at its origin, and this dilatation is called the superior bulb.
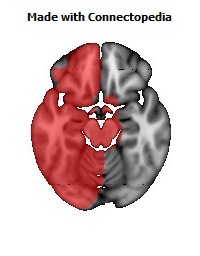
It also has a common trunk into which drains the anterior branch of the retromandibular vein, the facial vein, and the lingual vein.
It runs down the side of the neck in a vertical direction, being at one end lateral to the internal carotid artery, and then lateral to the common carotid, and at the root of the neck, it unites with the subclavian vein to form the brachiocephalic vein (innominate vein); a little above its termination is a second dilatation, the inferior bulb.
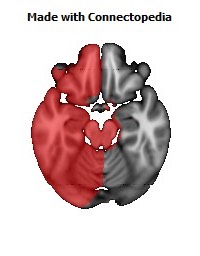
Above, it lies upon the rectus capitis lateralis, behind the internal carotid artery and the nerves passing through the jugular foramen; lower down, the vein and artery lie upon the same plane, the glossopharyngeal and hypoglossal nerves passing forward between them; the vagus descends between and behind the vein and the artery in the same sheath (the carotid sheath), and the accessory runs obliquely backward, superficial or deep to the vein.
At the root of the neck, the right internal jugular vein is a little distance from the common carotid artery, and crosses the first part of the subclavian artery, while the left internal jugular vein usually overlaps the common carotid artery.
The left vein is generally smaller than the right, and each contains a pair of valves, which are placed about 2.5 cm above the termination of the vessel.
Clinical relevance
The jugular veins are relatively superficial and not protected by tissues such as bone or cartilage. This makes them susceptible to damage. Due to the large volumes of blood that flow though the jugular veins, damage to the jugulars can quickly cause significant blood loss, which can lead to hypovolæmic shock and then death if not treated.
It should also be noted that cuts or abrasions in the skin near the jugular vein will bleed longer and more profusely (e.g. shaving accidents). Since 95% of the body's blood passes through this vein, it takes on average about 30 minutes to fully stop a shaving abrasion on the face.
JVP
As there is one pair of valves between the right atrium of the heart and the internal jugular, blood can flow back into the internal jugular when the pressure in the atrium is sufficiently high. This can be seen from the outside, and allows one to estimate the pressure in the atrium. The pulsation seen is called the jugular venous pressure, or JVP. This is normally viewed with the patient at 45 degrees turning his/her head slightly away from the observer. The JVP can be raised in a number of conditions:
- right ventricular failure (heart failure),
- tricuspid stenosis
- tricuspid regurgitation
- cardiac tamponade
The JVP can also be artificially raised by applying pressure to the liver (the hepatojugular reflux). This method is used to locate the JVP and distinguish it from the carotid pulse. Unlike the carotid pulse, the JVP is impalpable.
Catheterization
As the internal jugular is large, central and relatively superficial, it is often used to place venous lines. Such a line may be inserted for several reasons, such as to accurately measure the central venous pressure or to administer fluids when a line in a peripheral vein would be unsuitable (such as during resuscitation when peripheral veins are hard to locate).
Because the internal jugular rarely varies in its location, it is easier to find than other veins. However, sometimes when a line is inserted the jugular is missed and other structures such as the carotid artery or the vagus nerve (CN X) are punctured, and damage is caused to these structures.