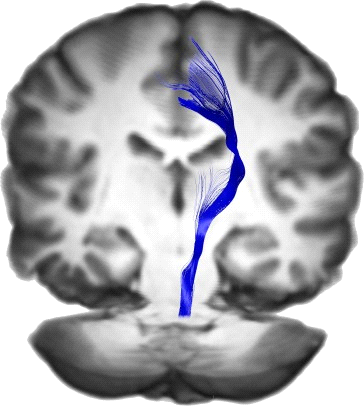
The pyramidal tracts refer to both the corticospinal and corticobulbar tracts of the nervous system.
The corticospinal tract conducts impulses from the brain to the spinal cord. It contains mostly axons originated from the motor cortex. The corticospinal tract is made up of two separate tracts in the spinal cord: the lateral corticospinal tract and the anterior corticospinal tract. The corticospinal tract also contains betz cells (the largest pyramidal cells), which are not found in any other region of the body. An understanding of these tracts leads to an understanding of why one side of the body is controlled by the opposite side of the brain. The corticospinal tract is concerned specifically with discrete voluntary skilled movements, such as precise movement of the fingers and toes. The brain sends impulses to the spinal cord relaying the message. This is imperative in understanding that the left hemisphere of the brain controls the right side of the body, while the right hemisphere of the brain controls the left side of the body. The tracts cross in the medulla oblongata in a process also known as decussation.
The corticobulbar tract carries information to motor neurons of the cranial nerve nuclei, rather than the spinal cord. These nerves control the muscles of the face and neck and are involved in facial expression, mastication, swallowing, and other functions.
Structure
Motor pathway
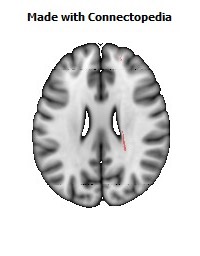
The corticospinal tract originates from pyramidal cells in layer V of the cerebral cortex. About 31% of its fibers arise from the primary motor cortex. Other contributions come from the supplementary motor area and the premotor cortex which constitute 29% of fibers while the somatosensory cortex, parietal lobe, and cingulate gyrus supplies the rest. The average fiber diameter is in the region of 10μm; around 3% of fibres are extra-large (20μm) and arise from Betz cells, mostly in the leg area of the primary motor cortex.
The neuronal cell bodies in the motor cortex, together with their axons that travel down through the brain stem and spinal cord are commonly referred to as upper motor neurons.
Decussation and synapses
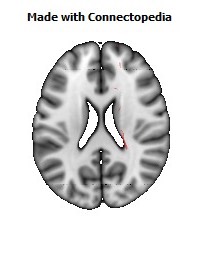
Some of the neuronal cell bodies in the motor cortex send long axons to the motor cranial nerve nuclei mainly of the contralateral side of the midbrain (cortico-mesencephalic tract), pons (Corticopontine tract), and medulla oblongata (cortico-bulbar tract), decussating just before they reach their target nuclei. These are called geniculate fibers. Many more motor cortex neurons, however, extend fibers all the way down to the spinal cord (corticospinal tract).
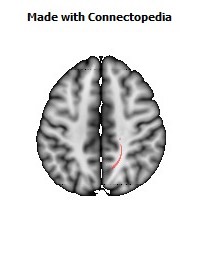
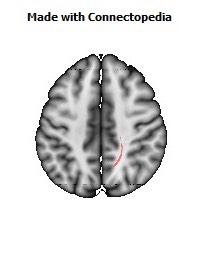
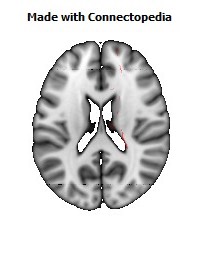
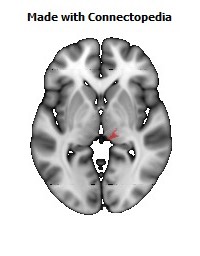
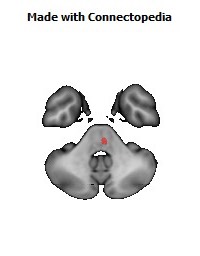
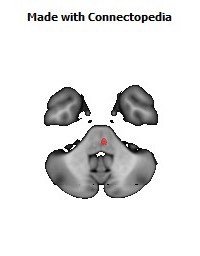
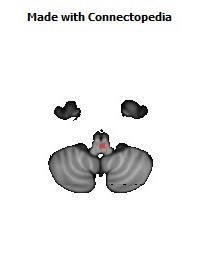
• Most of the corticospinal fibers (about 80%) cross over to the contralateral side in the medulla oblongata (pyramidal decussation). Those that cross in the medulla oblongata travel in the lateral corticospinal tract.
• 10% Enter the lateral corticospinal tract on the same side.
• The remainder of them (10%) travel in the anterior corticospinal tract. The majority of fibers from this tract cross over near the level that they exit the spinal cord, however a small portion will synapse in the anterior horn on the ipsilateral side.
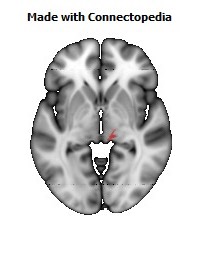
Whichever of these two tracts it travels in, a corticospinal axon will synapse with another neuron in the ventral horn. This ventral horn neuron is considered a second-order neuron in this pathway, but is not part of the corticospinal tract itself.
From cerebral to motor neurons
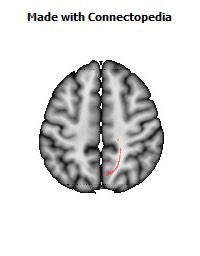
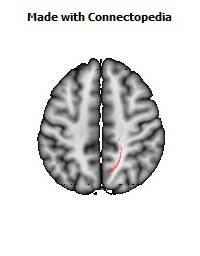
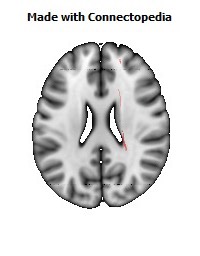
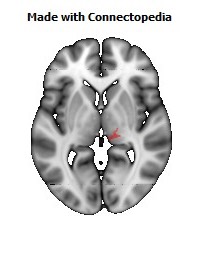
The motor axons move closer together as they travel down through the cerebral white matter, and form part of the posterior limb of the internal capsule.
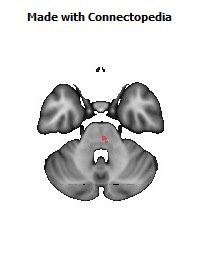
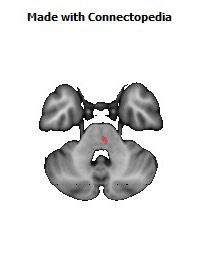
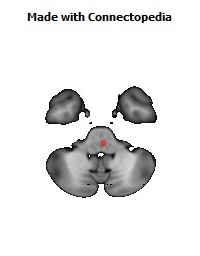
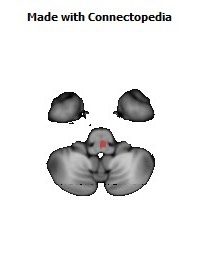
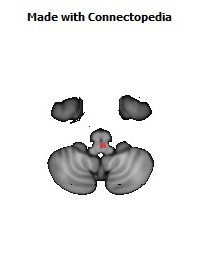
The motor fibers continue down into the brainstem. The bundle of corticospinal axons is visible as two column-like structures ("pyramids") on the ventral surface of medulla oblongata. However, the name pyramidal tract comes from the pyramidal/conical shape of the neuron cell bodies (soma) that comprise it.
After the decussation, the axons travel down the spinal cord as the lateral corticospinal tract. Fibers that do not cross over in the medulla oblongata travel down the separate anterior corticospinal tract, and most of them cross over to the contralateral side in the spinal cord, shortly before reaching the lower motor neurons.
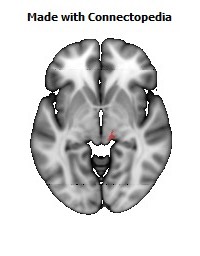
Lower motor neurons
In the spinal cord, the axons of the upper motor neuron connect (most of them via interneurons, but to a lesser extent also via direct synapses) with the lower motor neurons, located in the ventral horn of the spinal cord.
In the brain stem, the lower motor neurons are located in the motor cranial nerve nuclei (oculomotor, trochlear, motor nucleus of the trigeminal nerve, abducens, facial nerve, accessory, hypoglossal). The lower motor neuron axons leave the brain stem via motor cranial nerves and the spinal cord via anterior roots of the spinal nerves, respectively, ending up at the neuromuscular plate and providing motor innervation for voluntary muscles.
Sensory
• Spinothalamic tract
• Spinocerebellar tract
• Visual pathway
• Olfactory system
• Posterior column pathway
Neurons
The neurons of the these tracts are referred to as pyramidal tract neurons (PTN), because their axons form part of the pyramidal tracts leading to the spinal cord (or the cranial nerve nuclei with the corticobulbar tract), which in turn are named such because in cross-section they resemble pyramids as they pass through the medulla.
Pyramidal tract neurons, however, are not to be confused with pyramidal neurons: a super-class of neurons, found in many parts of the brain including the cerebral cortex and the hippocampus, whose name derives from the pyramid-like shape of the cell body (soma). In fact, corticospinal neurons are both pyramidal tract neurons (because their axons pass through the medullary pyramids) and pyramidal neurons (because their cell body is shaped like a pyramid).
Extrapyramidal motor pathways
In anatomy, the extrapyramidal system is a neural network that is part of the motor system that causes involuntary reflexes and movement, and modulation of movement (i.e. coordination). The system is called "extrapyramidal" to distinguish it from the tracts of the motor cortex that reach their targets by traveling through the "pyramids" of the medulla. The pyramidal pathways (corticospinal and some corticobulbar tracts) may directly innervate motor neurons of the spinal cord or brainstem (anterior (ventral) horn cells or certain cranial nerve nuclei), whereas the extrapyramidal system centers around the modulation and regulation (indirect control) of anterior (ventral) horn cells.
Extrapyramidal tracts are chiefly found in the reticular formation of the pons and medulla, and target neurons in the spinal cord involved in reflexes, locomotion, complex movements, and postural control. These tracts are in turn modulated by various parts of the central nervous system, including the nigrostriatal pathway, the basal ganglia, the cerebellum, the vestibular nuclei, and different sensory areas of the cerebral cortex. All of these regulatory components can be considered part of the extrapyramidal system, in that they modulate motor activity without directly innervating motor neurons.
The extrapyramidal system is very old and three of the four tracts of the human extrapyramidal system are clearly present in salamanders.
The extrapyramidal tracts include parts of the following:
- rubrospinal tract
- pontine reticulospinal tract
- medullary reticulospinal tract
- lateral vestibulospinal tract
- tectospinal tract
These are motor pathways that lie outside the corticospinal tract and are beyond voluntary control. Their main function is to support voluntary movement and help control posture and muscle tone.
Clinical significance
Damage to the descending motor pathways anywhere along the trajectory from the cerebral cortex to the lower end of the spinal cord gives rise to a set of symptoms called the "Upper Motor Neuron Syndrome". A few days after the injury to the upper motor neurons, a pattern of motor signs and symptoms appears, including spasticity, increased vigor (and decreased threshold) of deep tendon reflexes, a loss of the ability to perform fine movements, and an extensor plantar response known as the Babinski sign.